Pressure Ulcers
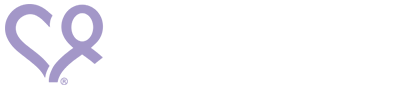
Pressure ulcers are wounds formed by unrelieved pressure on the skin and are usually over bony areas of the body such as the elbow, heels, hips, and shoulders. Pressure ulcers can happen if someone is sitting or lying for too long but can be prevented early on with proper measures in place. If pressure ulcers are not noticed right away, they can become painful and even infected. They are caused when the blood supply to the skin is reduced because too much pressure is placed for too long on the same area.
There are three primary reasons pressure ulcers happen:
- Pressure: Constant pressure on any part of the body especially bony areas.
- Friction: When the skin rubs against a stationary surface.
- Shear: Happens when you transfer a person, when they reach for something while sitting, or when they change positions. It can cause damage underneath the skin that often goes undetected until redness on the skin is visible.
Avoid friction on the person’s skin:
- Learn how to properly transfer a person with dementia to avoid dragging the skin. Ask your doctor to prescribe a visit from an occupational therapist or nurse to teach you how to do this.
- Make sure there are no rough seams on their clothing or anything in their pockets.
- Keep the bedsheets smooth; wrinkled sheets can cause pressure ulcers.
Use gentle motions when washing the skin and pat dry gently.
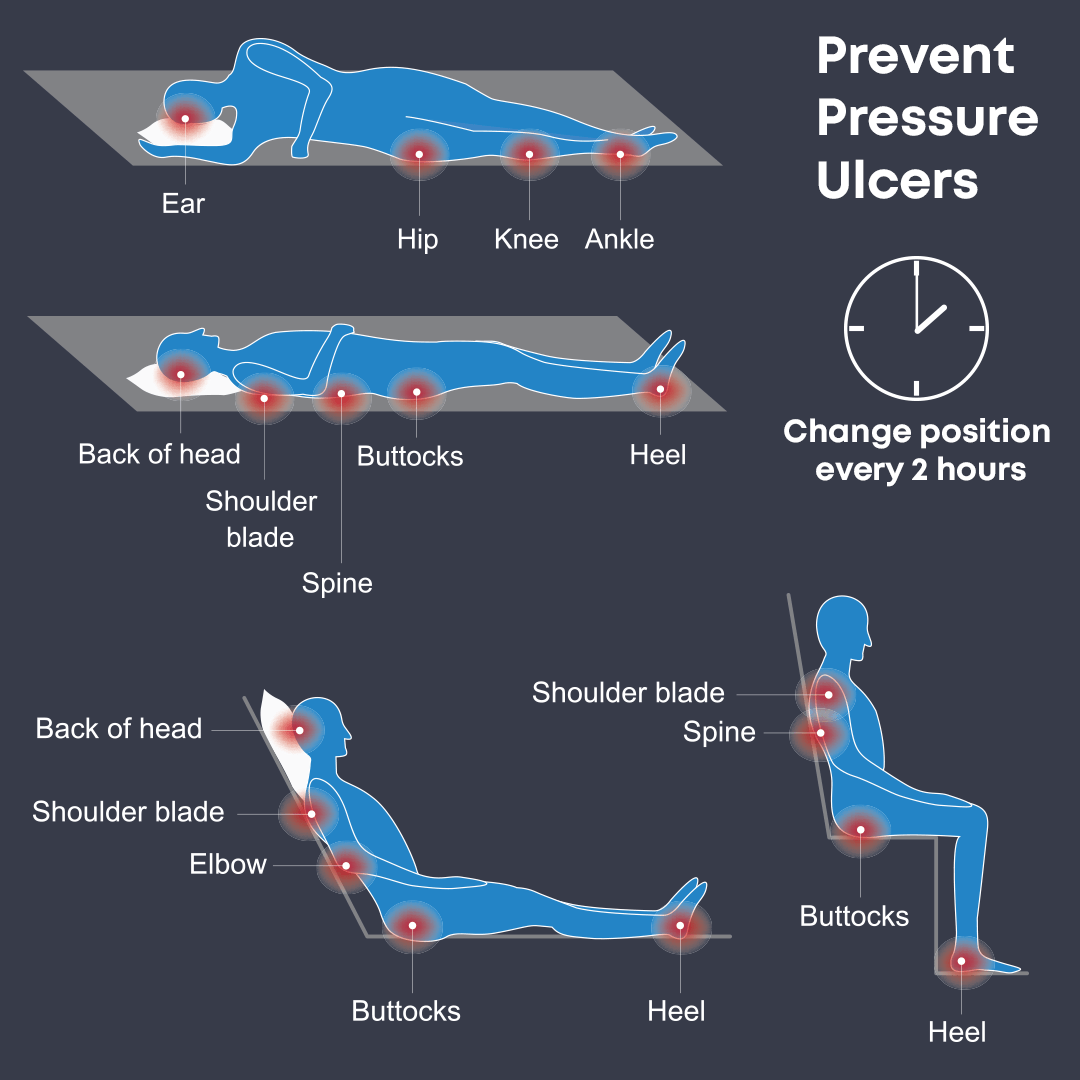
Stages of Pressure Ulcers
Stage 1: (least severe) Persistent redness of skin
Stage 2: Loss of partial thickness of the skin, appearing as an abrasion, blister, or shallow crater
Stage 3: Loss of full thickness of the skin, presenting as a deep crater
Stage 4: (most severe) Loss of full thickness of the skin, exposing muscle or bone
How to spot the signs of a pressure ulcer:
- If the person has red patches on their skin, press lightly with your finger. If it does not go away, this may be an early sign of a pressure ulcer.
- The affected area may be painful, hard, or hot to the touch.
- For people with darker skin, pressure ulcers may have a purple or blue tint.
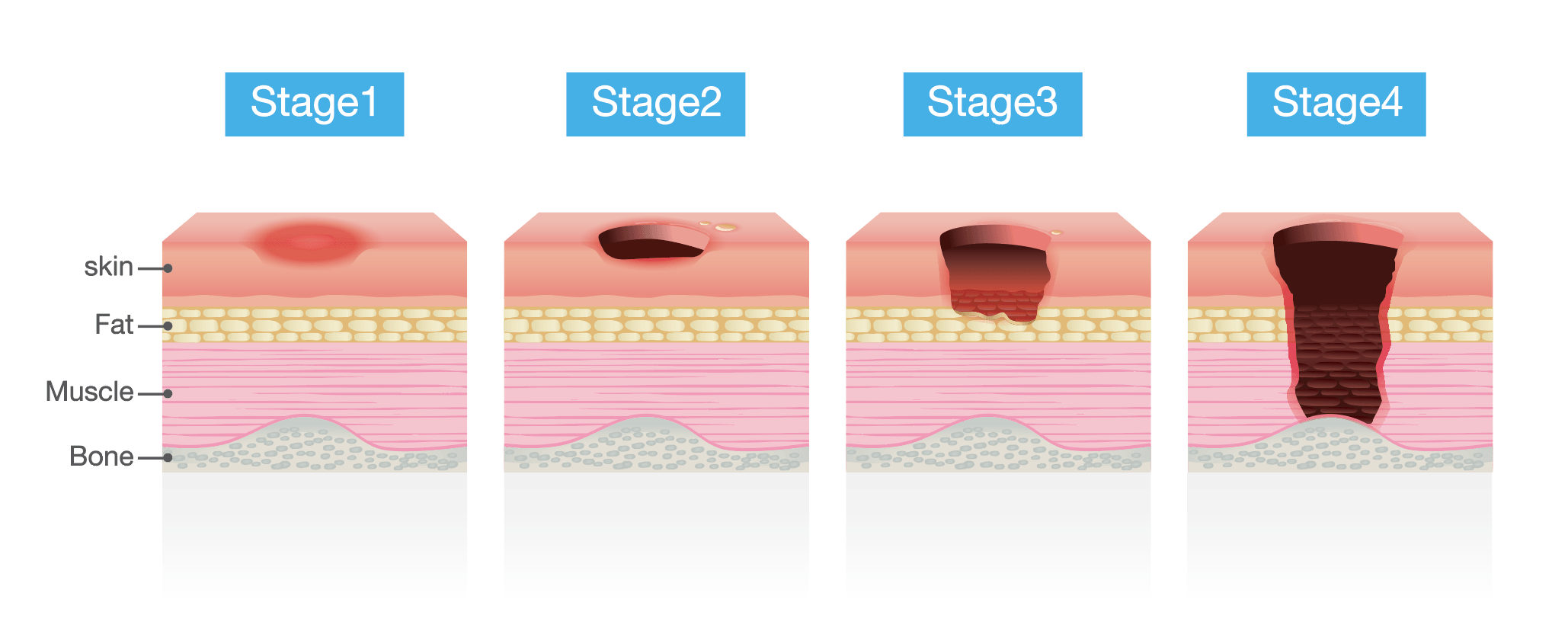
- Make sure you check the person’s skin frequently, especially on areas where there is regular pressure, like heels, ankles, knees, buttocks, hips, spine, elbows, shoulder blades, and the back of the head.
- If a pressure ulcer is spotted, contact the doctor right away.
Tips to avoid pressure ulcers:
- Chair-based exercises can help relieve pressure and improve blood flow.
- Make sure the person has a well-balanced diet. If they have trouble swallowing, ask for a referral to a speech therapist.
- If incontinence is a problem, make sure they do not stay in their wet clothes or bed for long periods of time.
- Avoid excessive heat or moisture.
- Avoid tight fitting clothing.
- After a bath, pat it dry; don’t rub the skin to dry it.
- Do not rub any places on the body that are red.
How to prevent pressure ulcers:
- While lying in bed:
- Change the person’s position or have them change their position every two hours.
- Encourage them to get up and move around even if it’s with help.
- Ask your doctor or nurse about pressure relieving pads, mattresses, or overlays.
- Position their body properly in bed to relieve pressure and improve blood flow.
- While sitting in chair or wheelchair:
- Encourage them to change their position in the chair every 15-30 minutes to relieve pressure on each side.
- Have the person walk around periodically, if it is safe.
- Use pressure relieving seat cushions on chairs and wheelchairs.